Diabetes and the Eye
Diabetes Mellitus has been diagnosed in over 14 million individuals in the United States. There are two basic forms of diabetes. Type II diabetes or non-insulin dependent diabetes (NIDDM) is also known as adult onset diabetes. It is most typically diagnosed in adults who tend to be overweight. Type II diabetes is most typically treated with oral medications; however a significant number of these individuals do require insulin therapy.
A more severe form of diabetes is termed Type I diabetes, or insulin dependent diabetes. Also known as juvenile onset diabetes, this form tends to require insulin therapy. Although eye complications can be found with both forms of diabetes, Type I diabetes has more frequent and severe ocular complications.
Eye Complications of Diabetes
There are numerous complications that can occur in the eye secondary to diabetes, some of which are mild, insignificant, or transient and others of which are severe and vision threatening. Diabetes is the leading cause of blindness among patients under the age of 65. Eye complications of diabetes include:
- Significant and sudden shifts in vision prescription (large increases in nearsightedness or farsightedness). This is associated with changes in blood sugar levels and its effect on the focusing lens of the eye.
- Acute diplopia (double vision). Double vision associated with diabetes tends to be binocular (one of the two images will go away if you close or cover one eye). It tends to be transient, lasting generally days to weeks at most. It is due to compromised blood flow to the nerves that control the external eye musles.
- Cataract development. Cataracts tend to develop earlier and more significantly in people with diabetes.
- Glaucoma. Diabetes is a relative risk factor for the development of glaucoma. A rare, but very severe form of glaucoma called “neovascular glaucoma” is found in advanced diabetics.
- Diabetic Retinopathy is the most feared complication of diabetes.
What is Diabetic Retinopathy?
Diabetic retinopathy is a term used to describe consequences of abnormalities in the blood vessels of the retina that occur in diabetes. There are basically two forms of diabetic retinopathy, “Background” and “Proliferative.”
 Background diabetic retinopathy by far is the most common and least severe form. It involves bleeding within the various layers of the retina (hemorrhages) and leakage of serum into the retina which results in protein deposits called “exudates”. This form of retinopathy typically does not cause any vision loss, but may be a precursor to proliferative retinopathy. Should fluid leak into the central retina called the “macula”, then central vision is threatened. This condition is termed diabetic macula edema.
Background diabetic retinopathy by far is the most common and least severe form. It involves bleeding within the various layers of the retina (hemorrhages) and leakage of serum into the retina which results in protein deposits called “exudates”. This form of retinopathy typically does not cause any vision loss, but may be a precursor to proliferative retinopathy. Should fluid leak into the central retina called the “macula”, then central vision is threatened. This condition is termed diabetic macula edema.
Proliferative diabetic retinopathy occurs when the retina is not receiving enough oxygen due to the severity of the background retinopathy. In response to this inadequate level of retinal oxygenation (or “hypoxia”) a vasoactive substance is produced which stimulates the production of new retinal vessels called “neovascular vessels”. These new vessels are very fragile and tend to bleed and leak profusely. Severe bleeds can enter the vitreous or pre-retina space and severely effect vision. These large bleeds may require surgery to remove the blood. Over time the new vessels form fibrous connective tissue bands that create traction to the retina and can lead to a very special form of retinal detachment.
Although some complications of diabetic eye disease cause symptoms, many do not, especially in their early phases. There are very specific clinical findings that indicate the need for treatment. A detailed retinal examination by your doctors at Krzyzak Eyecare will determine your condition and treatment.
Treatment of Diabetic Retinopathy
 The most critical aspect of treatment for diabetic eye complications involves the tight control of the disease itself. This relates to tight control of blood sugar levels, weight, and blood pressure. This is crucial in the prevention of ocular complications in diabetes as well as in slowing the progression of the disease.
The most critical aspect of treatment for diabetic eye complications involves the tight control of the disease itself. This relates to tight control of blood sugar levels, weight, and blood pressure. This is crucial in the prevention of ocular complications in diabetes as well as in slowing the progression of the disease.
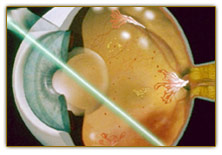
Laser retinal therapy is the mainstay of specific treatment for diabetic retinopathy. Laser therapy is used in one of two ways for retinopathy. First focal laser treatment is used to seal specific areas of blood vessel leakage. This is especially useful if macula edema is due to a localized area of leakage.
 Occasionally the macula edema is more diffuse and a “grid pattern” of laser is used. In cases of proliferative diabetic retinopathy a form of laser therapy known as “pan retinal photocoagulation” (PRP) is used. In this case large areas of under-oxygenated retina are treated with a scatter of many laser burns. The destruction of this already damaged retina reduces the oxygen demand of the retina as a whole, thus reducing the stimulus to create new fragile neovascular vessels.
Occasionally the macula edema is more diffuse and a “grid pattern” of laser is used. In cases of proliferative diabetic retinopathy a form of laser therapy known as “pan retinal photocoagulation” (PRP) is used. In this case large areas of under-oxygenated retina are treated with a scatter of many laser burns. The destruction of this already damaged retina reduces the oxygen demand of the retina as a whole, thus reducing the stimulus to create new fragile neovascular vessels.
PRP is destructive in nature and not intended to improve vision per se. the goal of PRP is to prevent further vision loss and potentially blinding complications of diabetic retinopathy. Following PRP there can be some loss of side vision and color vision in some cases. All laser treatments for diabetic retinopathy are performed as an outpatient procedure and do not require hospitalization.
Vitrectomy surgery is a complex eye operation that is used to remove persistent vitreous hemorrhage and to treat tractional retinal detachments. It is only performed by highly specialized retinal specialists and is done in the hospital.
